Medical
The military medical technology saving lives on the front line
Administering fast and effective first aid on the front line is a matter of life and death and having access to cutting-edge combat-compatible medical technology can make all the difference. Heidi Vella takes a look at some innovations being advanced for the military today.
The provision of front line medical care has improved drastically over the last decade.
Yet, with the military’s special requirements for technologies to be lightweight, portable and so-called ‘soldier-proof’ – because they may need to be administered by non-medical professionals – gaps in care persist or solutions could be improved further.
Stemming blood loss and administering transfusions, clearing airways and facilitating fast evacuation are all procedures of paramount importance. Even small technological advancements in these areas can save lives. Analysis of all US military casualties from October 2001 through December 2017 found that survival among the most critically injured casualties increased three-fold due to improvements in methods to control bleeding, replace blood and reduce time to treatment.
Fortunately, research and development continues apace to find better, more efficient solutions that work well even in the remote, austere and unsanitary environments the military often operates in.
Preventing excessive bleeding
Haemorrhaging is a leading cause of preventable death for soldiers in combat. This is particularly acute for non-compressible areas, such as the groin, trunk, armpit, neck and internal organs, as compression packs routinely carried by soldiers don’t work on these types of bleed.
We want to make sure an average person with very limited training could apply this and it would have efficacy
To solve this problem, researchers are developing a new type of liquid, called Statbond, that could be put directly onto a wound without the need for compression to stop or slow bleeding long enough for the patient to reach a hospital. Based on visco-liquid haemostatic agents, which can penetrate deep into a wound and seal against fluid loss, the technology helps natural blood-clotting cascade to happen against the surface of the gel.
“This is particularly important for injuries to arteries which are linked directly to the heart and pulse, interfering with clot formation,” explains Dr Robert Mantz, a chemistry branch chief with the Army Research Lab, which is developing the technology with Hybrid Plastics, the University of Mississippi Medical Center, Vanderbilt University and Ichor Sciences.
The solution, which recently completed successful animal studies, is currently undergoing a phase II enhancement study and FDA registration. It’s expected to be available for physicians in 2022 and potentially carried by soldiers in the form of a durable pocket-carry squeeze pack by 2025.
“We want to make sure an average person with very limited training could apply this and it would have efficacy,” adds Mantz.
Also addressing blood loss, in the UK researchers at the University of Bristol are looking at ways to make blood transfusions during combat easier. They’re conducting trials on how to ‘grow’ and mature red blood cells in the laboratory with funding from the government’s Defence Science and Technology Laboratory.
This manmade blood could potentially be administered to anyone, regardless of their blood type, and freeze-dried for easy storage and transportation. This would be especially useful in combat situations, considering seven years of British ops in Afghanistan saw around 15,500 litres of blood transfused to 2,600 patients. However, trials are in the early stages and could take a decade to develop.

// Simon Galt is Aurora managing director at QinetiQ about what this means for accelerating defence innovation. Credit: QinetiQ
Life and breath
If a combat soldier sustains a lung injury, medics have mere minutes to intervene to support their lung function. A new chest tube system, which became commercially available in June, hopes to help front line first aiders quickly relieve symptoms of air and fluid in the lungs that can restrict breathing.
The Quick Tube system can be inserted into a patient to support their breathing in a ‘record-setting’ 30 to 45 seconds, according to its creators, Quick Tube Medical. This is compared with up to eight minutes for traditional chest tubes, which require incisions.
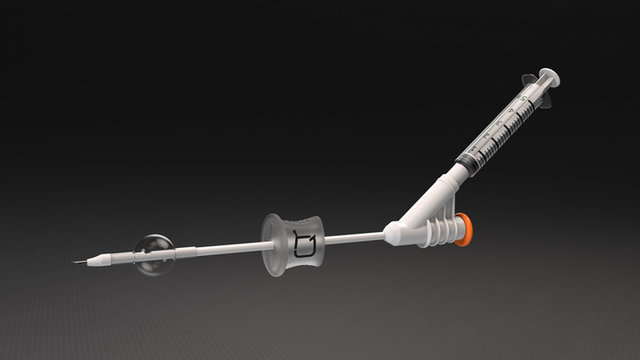
// The Quick Tube system helps front line first aiders quickly relieve symptoms of air and fluid in the lungs. Credit: Quick Tube Madical
The flexible plastic chest tube is inserted through the chest wall and into the pleural space or mediastinum to remove air pneumothorax and/or fluid, such as blood or mucus. Its specially-shaped nib allows for quick entry into the flesh and organ.
“Oftentimes, these types of procedures need to be done outside a clinic or a hospital setting. The Quick Tube needs no initial incision or suturing, resulting in a quick and effective procedure in all environments,” says Charles Pollak, president at Red One Medical, a US government contractor. The company has partnered with Quick Tube Medical to deliver the FDA-registered standardised chest tube system to the US army.
A nascent but burgeoning trend in military medical technology combat interventions that could eventually assist with the use of tools such as the Quick Tube is telemedicine. For around 18 months, the British Army has been experimenting with using augmented reality for medics under a programme codenamed Project Lara.
The Royal Army Medical Corps plans for the technology to provide junior medics in the field with access to advice and expertise from specialised paramedics located elsewhere. The more experienced medic will follow the operation remotely and provide instructions via Microsoft HoloLens 2 augmented reality spectacles, which could help junior medics conduct procedures such as the insertion of the chest tube system.
Preventing infection
If left untreated, the risk from infected cuts and wounds can be equally as deadly as other more immediately serious injuries. A possible front-line friendly solution to combat infection is being developed by scientists in Sweden. Researchers at Chalmers University of Technology, in collaboration with Amferia, have created an easy-to-apply hydrogel that works to prevent infection from all types of bacteria, including antibiotic-resistant ones.

// Chalmers University of Technology researchers have developed a nanostructured hydrogel to prevent infections. Credit: Anna-Lena Lundqvist / Chalmers
The hydrogel is made of a new bactericidal material that consists of antimicrobial peptides, which are small proteins found naturally in the immune system. Normally these peptides can be broken down quickly by enzymes in blood and so lose their potency. However, the nanostructured hydrogel, into which the peptides are permanently bound, create a protective environment, preserving their effectiveness. Ongoing studies have shown it has a high level of effectiveness against bacteria.
It wasn’t designed for the military specifically, but has clear usage potential on the front line, according to head researcher of the study and founder of Amferia, Martin Andersson.
“If you don't have access to clean hospital equipment you can apply these patches directly onto the wound as a way of preventing a severe infection later on,” explains Andersson. “This will be especially effective in an area, such as Southern Europe or Asia, where antibiotic-resistant bacteria are more common.”
Fast evacuation
Once emergency first aid has been administered and a wounded combatant is stabilised, facilitating fast evacuation within the so-called ‘golden hour’, in which it is most likely medical intervention will prevent death, is the next step in saving their life.
This can increase the likelihood of the wounded person surviving
Autonomous vehicles, such as those developed by Milrem Robotics, can do this three times faster than two soldiers carrying a wounded person on a stretcher, according to Jüri Pajuste, defence research and development director at Milrem Robotics. “This can increase the likelihood of the wounded person surviving,” he explains.
The company’s THeMIS Combat Support unmanned ground vehicle can transport up to three wounded soldiers on stretchers, meaning manpower can be freed up.
“The UGV gives you a certain flexibility because you don’t need to use many soldiers to carry the wounded and you can keep more fighting power where it’s needed,” adds Pajuste, who is also a reservist Estonian Defence Forces Captain.
THeMIS Combat Support was trialled in April by the Estonian Defence Forces Artillery Battalion in a live-fire exercise, during which they successfully removed an ‘injured’ soldier from the battlefield. Its hybrid-electric power system means it can stay on a mission for up to 24 hours or longer if extra fuel is carried. It can also be equipped with light remote weapon systems to increase firepower.
Though not commonly used in combat situations today, Pajuste believes the multiple applications and benefits of UGVs, including for casualty evacuation, will see the technology adopted more widely in future.
// Main image: Stopping bleeding rapidly saves lives on the battlefield. Credit: US Army